EXHIBIT 99.1
Published on July 18, 2025
|
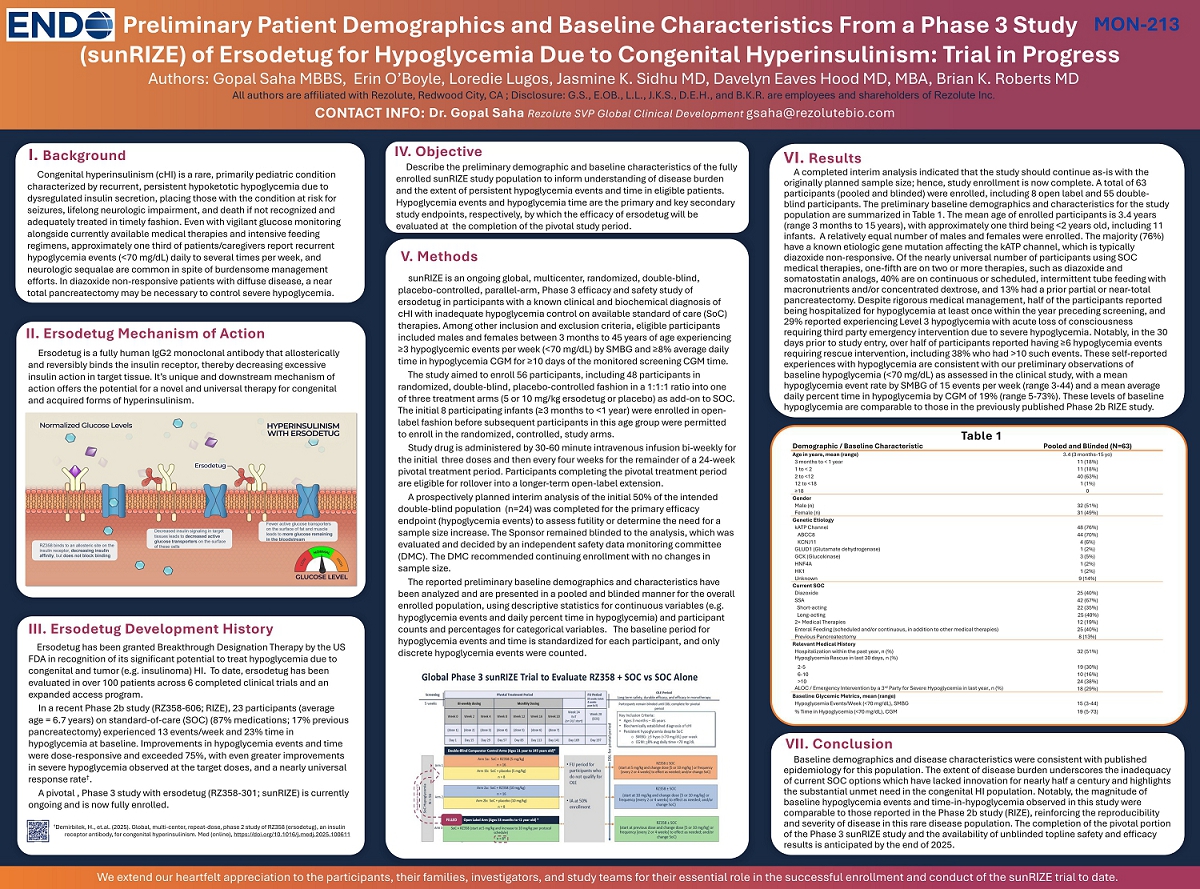
Baseline demographics and disease characteristics were consistent with published epidemiology for this population. The extent of disease burden underscores the inadequacy of current SOC options which have lacked innovation for nearly half a century and highlights the substantial unmet need in the congenital HI population. Notably, the magnitude of baseline hypoglycemia events and time-in-hypoglycemia observed in this study were comparable to those reported in the Phase 2b study (RIZE), reinforcing the reproducibility and severity of disease in this rare disease population. The completion of the pivotal portion of the Phase 3 sunRIZE study and the availability of unblinded topline safety and efficacy results is anticipated by the end of 2025. A completed interim analysis indicated that the study should continue as-is with the originally planned sample size; hence, study enrollment is now complete. A total of 63 participants (pooled and blinded) were enrolled, including 8 open label and 55 double-blind participants. The preliminary baseline demographics and characteristics for the study population are summarized in Table 1. The mean age of enrolled participants is 3.4 years (range 3 months to 15 years), with approximately one third being <2 years old, including 11 infants. A relatively equal number of males and females were enrolled. The majority (76%) have a known etiologic gene mutation affecting the kATP channel, which is typically diazoxide non-responsive. Of the nearly universal number of participants using SOC medical therapies, one-fifth are on two or more therapies, such as diazoxide and somatostatin analogs, 40% are on continuous or scheduled, intermittent tube feeding with macronutrients and/or concentrated dextrose, and 13% had a prior partial or near-total pancreatectomy. Despite rigorous medical management, half of the participants reported being hospitalized for hypoglycemia at least once within the year preceding screening, and 29% reported experiencing Level 3 hypoglycemia with acute loss of consciousness requiring third party emergency intervention due to severe hypoglycemia. Notably, in the 30 days prior to study entry, over half of participants reported having ≥6 hypoglycemia events requiring rescue intervention, including 38% who had >10 such events. These self-reported experiences with hypoglycemia are consistent with our preliminary observations of baseline hypoglycemia (<70 mg/dL) as assessed in the clinical study, with a mean hypoglycemia event rate by SMBG of 15 events per week (range 3-44) and a mean average daily percent time in hypoglycemia by CGM of 19% (range 5-73%). These levels of baseline hypoglycemia are comparable to those in the previously published Phase 2b RIZE study. sunRIZE is an ongoing global, multicenter, randomized, double-blind, placebo-controlled, parallel-arm, Phase 3 efficacy and safety study of ersodetug in participants with a known clinical and biochemical diagnosis of cHI with inadequate hypoglycemia control on available standard of care (SoC) therapies. Among other inclusion and exclusion criteria, eligible participants included males and females between 3 months to 45 years of age experiencing ≥3 hypoglycemic events per week (<70 mg/dL) by SMBG and ≥8% average daily time in hypoglycemia CGM for ≥10 days of the monitored screening CGM time. The study aimed to enroll 56 participants, including 48 participants in randomized, double-blind, placebo-controlled fashion in a 1:1:1 ratio into one of three treatment arms (5 or 10 mg/kg ersodetug or placebo) as add-on to SOC. The initial 8 participating infants (≥3 months to <1 year) were enrolled in open-label fashion before subsequent participants in this age group were permitted to enroll in the randomized, controlled, study arms. Study drug is administered by 30-60 minute intravenous infusion bi-weekly for the initial three doses and then every four weeks for the remainder of a 24-week pivotal treatment period. Participants completing the pivotal treatment period are eligible for rollover into a longer-term open-label extension. A prospectively planned interim analysis of the initial 50% of the intended double-blind population (n=24) was completed for the primary efficacy endpoint (hypoglycemia events) to assess futility or determine the need for a sample size increase. The Sponsor remained blinded to the analysis, which was evaluated and decided by an independent safety data monitoring committee (DMC). The DMC recommended continuing enrollment with no changes in sample size. The reported preliminary baseline demographics and characteristics have been analyzed and are presented in a pooled and blinded manner for the overall enrolled population, using descriptive statistics for continuous variables (e.g. hypoglycemia events and daily percent time in hypoglycemia) and participant counts and percentages for categorical variables. The baseline period for hypoglycemia events and time is standardized for each participant, and only discrete hypoglycemia events were counted. Congenital hyperinsulinism (cHI) is a rare, primarily pediatric condition characterized by recurrent, persistent hypoketotic hypoglycemia due to dysregulated insulin secretion, placing those with the condition at risk for seizures, lifelong neurologic impairment, and death if not recognized and adequately treated in timely fashion. Even with vigilant glucose monitoring alongside currently available medical therapies and intensive feeding regimens, approximately one third of patients/caregivers report recurrent hypoglycemia events (<70 mg/dL) daily to several times per week, and neurologic sequalae are common in spite of burdensome management efforts. In diazoxide non-responsive patients with diffuse disease, a near total pancreatectomy may be necessary to control severe hypoglycemia. I. Background V. Methods VI. Results VII. Conclusion Preliminary Patient Demographics and Baseline Characteristics From a Phase 3 Study (sunRIZE) of Ersodetug for Hypoglycemia Due to Congenital Hyperinsulinism: Trial in Progress Dr. Gopal Saha Rezolute SVP Global Clinical Development gsaha@rezolutebio.com Authors: Gopal Saha MBBS, Erin O’Boyle, Loredie Lugos, Jasmine K. Sidhu MD, Davelyn Eaves Hood MD, MBA, Brian K. Roberts MD All authors are affiliated with Rezolute, Redwood City, CA ; Disclosure: G.S., E.OB., L.L., J.K.S., D.E.H., and B.K.R. are employees and shareholders of Rezolute Inc. CONTACT INFO: MON-213 Describe the preliminary demographic and baseline characteristics of the fully enrolled sunRIZE study population to inform understanding of disease burden and the extent of persistent hypoglycemia events and time in eligible patients. Hypoglycemia events and hypoglycemia time are the primary and key secondary study endpoints, respectively, by which the efficacy of ersodetug will be evaluated at the completion of the pivotal study period. IV. Objective Ersodetug is a fully human IgG2 monoclonal antibody that allosterically and reversibly binds the insulin receptor, thereby decreasing excessive insulin action in target tissue. It’s unique and downstream mechanism of action offers the potential for a novel and universal therapy for congenital and acquired forms of hyperinsulinism. II. Ersodetug Mechanism of Action Fewer active glucose transporters on the surface of fat and muscle leads to more glucose remaining in the bloodstream RZ358 binds to an allosteric site on the insulin receptor, decreasing insulin affinity, but does not block binding Decreased insulin signaling in target tissues leads to decreased active glucose transporters on the surface of these cells Ersodetug has been granted Breakthrough Designation Therapy by the US FDA in recognition of its significant potential to treat hypoglycemia due to congenital and tumor (e.g. insulinoma) HI. To date, ersodetug has been evaluated in over 100 patients across 6 completed clinical trials and an expanded access program. In a recent Phase 2b study (RZ358-606; RIZE), 23 participants (average age = 6.7 years) on standard-of-care (SOC) (87% medications; 17% previous pancreatectomy) experienced 13 events/week and 23% time in hypoglycemia at baseline. Improvements in hypoglycemia events and time were dose-responsive and exceeded 75%, with even greater improvements in severe hypoglycemia observed at the target doses, and a nearly universal response rate†. A pivotal , Phase 3 study with ersodetug (RZ358-301; sunRIZE) is currently ongoing and is now fully enrolled. III. Ersodetug Development History †Demirbilek, H., et.al. (2025). Global, multi-center, repeat-dose, phase 2 study of RZ358 (ersodetug), an insulin receptor antibody, for congenital hyperinsulinism. Med (online), https://doi.org/10.1016/j.medj.2025.100611 Demographic / Baseline Characteristic Pooled and Blinded (N=63) Age in years, mean (range) 3.4 (3 months-15 yo) 3 months to < 1 year 11 (18%) 1 to < 2 11 (18%) 2 to <12 40 (63%) 12 to <18 1 (1%) ≥18 0 Gender Male (n) 32 (51%) Female (n) 31 (49%) Genetic Etiology kATP Channel 48 (76%) ABCC8 44 (70%) KCNJ11 4 (6%) GLUD1 (Glutamate dehydrogenase) 1 (2%) GCK (Glucokinase) 3 (5%) HNF4A 1 (2%) HK1 1 (2%) Unknown 9 (14%) Current SOC Diazoxide 25 (40%) SSA 42 (67%) Short-acting 22 (35%) Long-acting 25 (40%) 2+ Medical Therapies 12 (19%) Enteral Feeding (scheduled and/or continuous, in addition to other medical therapies) 25 (40%) Previous Pancreatectomy 8 (13%) Relevant Medical History Hospitalization within the past year, n (%) 32 (51%) Hypoglycemia Rescue in last 30 days, n (%) 2-5 19 (30%) 6-10 10 (16%) >10 24 (38%) ALOC / Emergency Intervention by a 3rd Party for Severe Hypoglycemia in last year, n (%) 18 (29%) Baseline Glycemic Metrics, mean (range) Hypoglycemia Events/Week (<70 mg/dL), SMBG 15 (3-44) % Time in Hypoglycemia (<70 mg/dL), CGM 19 (5-73) Table 1 We extend our heartfelt appreciation to the participants, their families, investigators, and study teams for their essential role in the successful enrollment and conduct of the sunRIZE trial to date. |